Introduction
Immunotherapy has started to transform bladder cancer treatment, but durable responses remain the exception rather than the rule. Understanding why requires models that capture the tumour microenvironment, not just tumour growth. This blog explores how the MB49 syngeneic bladder cancer model – across subcutaneous, orthotopic, MB49-luc, and metastatic formats – dissects myeloid-dominated “cold” TMEs, neutrophil-driven immune escape, BCG response, and PD-L1-dependent checkpoint timing.
Bladder cancer is clinically heterogeneous and notoriously difficult to treat once it progresses to muscle-invasive disease. Immune checkpoint blockade and intravesical immunotherapy have transformed parts of the treatment landscape. Yet durable responses remain limited to a subset of patients. The field therefore relies on robust preclinical models that recapitulate tumour-immune interactions and reveal why therapies succeed or fail.
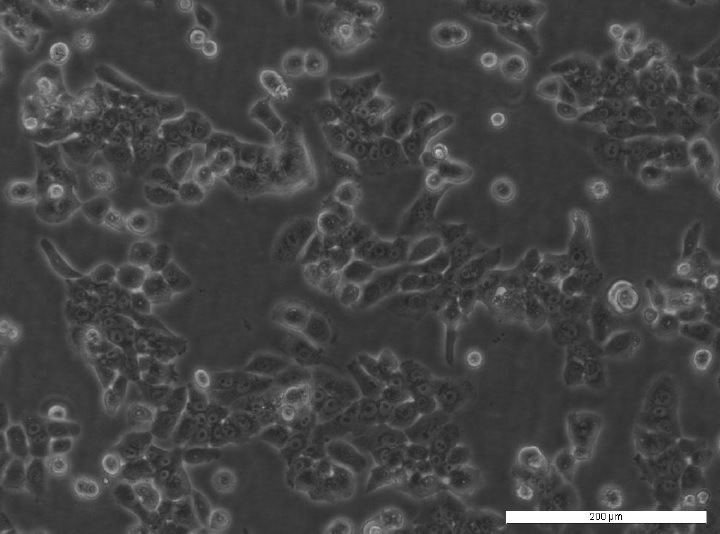
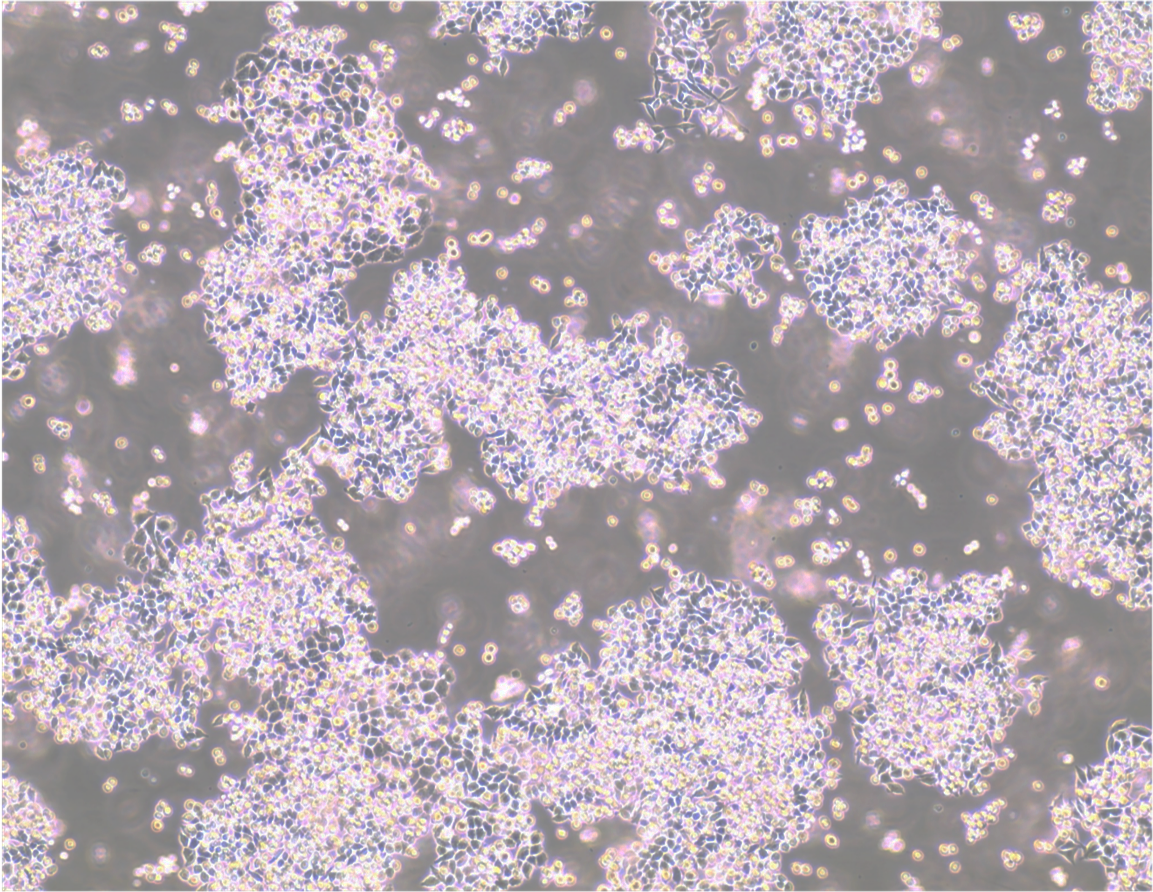
Among these, MB49 has emerged as one of the most reliable and informative models. Originally derived from chemically induced urothelial carcinoma arising in C57BL/ICRF-a(t) mouse bladder epithelium (1), MB49 has become a workhorse for studying the bladder tumour microenvironment (TME) and its manipulation by immunotherapy.

Image: Light microscope image of MB49 cells
What makes MB49 so valuable for bladder cancer research?
Its value lies in the combination of syngeneity and biological relevance (2–6):
- Reliable growth in immunocompetent models: MB49 grows readily in C57BL/6‑background mice, allowing studies in the context of intact host immunity (2–6).
- Epithelial, urothelial origin: The line is derived from chemically induced urothelial carcinoma and therefore recapitulates the epithelial nature of human bladder cancer (1).
- Clinically relevant antigen and checkpoint expression: MB49 expresses key molecules such as PD‑L1 and chemokines that are central to current immunotherapy strategies (1,4–6).
- Myeloid‑dominated, “cold” tumour microenvironment: Orthotopic MB49 tumours show a TME rich in suppressive myeloid cells with comparatively sparse T‑cell infiltration, closely resembling many human bladder tumours (2,4–6).
This “immunologically cold” phenotype mirrors a large fraction of human bladder tumours. MB49 therefore excels at dissecting immune evasion, myeloid–tumour crosstalk, and heterogeneous immunotherapy responses (2,4–7). Over the past two decades, MB49 underpins some of the clearest mechanistic insights into how the bladder TME becomes hostile to anti-tumour immunity, and how that state might be reversed. This impact is reinforced by MB49’s flexibility across multiple in vivo formats.
Choosing the right MB49 model
Researchers use MB49 in four main in vivo formats, each offering a slightly different window onto the TME and different practical advantages; subcutaneous, orthotopic, MB49-luc, and metastatic models (Table 1).
Subcutaneous MB49 tumours grow quickly and reproducibly, enabling clean readouts of tumour volume alongside rich TME profiling, ideal for dissecting innate pathways, macrophage polarisation, and checkpoint‑modulating therapies (3).
Orthotopic MB49 tumours, generated by intravesical instillation into pre‑injured bladders, add bladder‑specific factors such as urothelium, urine contact, and organ‑specific immune recruitment. This makes orthotopic models particularly powerful for intravesical BCG, gene therapy, and bladder‑targeted immunotherapy studies (3).
MB49-luc, a luciferase-tagged derivative of parental MB49 instilled orthotopically, enables longitudinal imaging and real-time TME tracking. Perfect for studying PD-L1 kinetics and therapy timing (4).
Metastatic MB49 models, typically generated via intravenous injection, extend investigations to distant immune niches, commonly the lung. These models excel at studying systemic immunity and dissemination (3).
| Model type | Setup | Best Use Case | Advantages | Disadvantages |
| Subcutaneous | MB49 cells injected under the skin (flank or hind leg) | Rapid efficacy and dosing studies; general TME and immune‑modulation; combo immunotherapy | Technically simple; highly reproducible; easy tumour measurement and tissue access | TME is skin/subcutis, not bladder; lacks urine exposure and bladder‑specific stromal context |
| Orthotopic | MB49 cells instilled into the bladder via catheter after urothelial pre‑injury | Bladder‑specific TME, intravesical BCG or gene therapy, modelling NMIBC progression | Anatomically and physiologically closest to human bladder cancer; native bladder microenvironments | Technically demanding; variable take; tumour monitoring often needs imaging or defined endpoints |
| MB49-luc (orthotopic) | Luciferase-tagged MB49 cells instilled intravesically | Longitudinal TME tracking; PD-L1 kinetics; intravesical therapy timing | Non-invasive bioluminescence imaging; temporal immune dynamics | Requires imaging equipment; luciferase signal variability |
| Metastatic | MB49 cells delivered IV (tail vein) | Metastatic spread, lung TME, systemic immunotherapy and adoptive cell therapy | Models dissemination and distant‑organ TME; suited to systemic therapy readouts | Primary tumour not in bladder; metastatic organ context differs; quantification more laborious |
Table 1: MB49 in vivo model formats – use cases and recommendations (3,4).
MB49 in action: neutrophils as architects of immune escape
One of the clearest examples of MB49’s translational impact comes from its role in understanding the function of neutrophils in bladder cancer. Clinically, high neutrophil infiltration has long been associated with poor prognosis (7), but the causality and mechanism were unclear.
Using orthotopic MB49 models, Jing et al. demonstrated that tumour-derived CXCL1, a major murine functional analogue of human IL-8, drives robust neutrophil recruitment into the bladder TME (7). Once present, these neutrophils secrete hepatocyte growth factor (HGF). This activates MET signalling in tumour cells and amplifies CXCL1 production. This results in a self-reinforcing, pro-tumour feedback loop.
Single-cell RNA sequencing resolved a distinct neutrophil subset characterised by high CCL3 and PD-L1 expression. This subset can suppress CD8⁺ T-cell proliferation and cytotoxicity (7). Functionally, disrupting this axis via CXCR1/2 blockade, inhibition of HGF–MET signalling, or combination with anti-PD-1 therapy restored T-cell activity and constrained tumour growth in MB49 models.
Importantly, the same IL-8–neutrophil–PD-L1 axis is evident in human bladder cancer, where elevated IL-8 correlates with neutrophil-rich, checkpoint-resistant disease. Urinary IL-8 and CCL3 have therefore emerged as promising non-invasive biomarkers for patient stratification, underscoring how MB49 can illuminate clinically actionable biology (7).
Beyond neutrophil biology, MB49 has also helped untangle the immune mechanisms underlying response and resistance to bladder cancer therapies.
Resolving BCG’s clinical paradox with MB49
The BCG (Bacillus Calmette‑Guérin) vaccine remains one of the earliest and most successful cancer immunotherapies, yet around 40% of patients with non‑muscle‑invasive bladder cancer fail to respond (8). MB49 helps explain why.
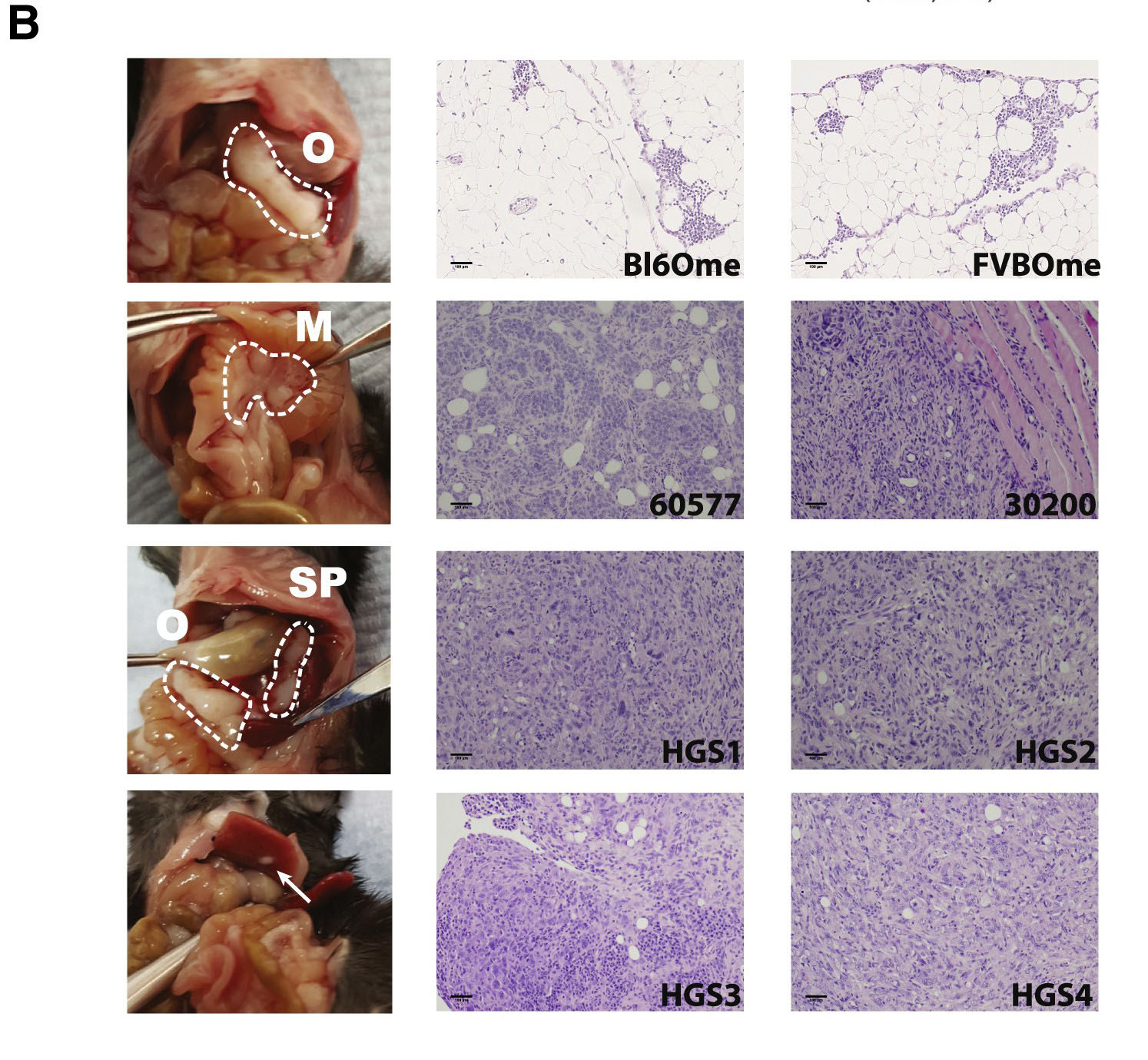
Using subcutaneous MB49 tumours implanted into genetically defined mouse strains, de Queiroz and colleagues showed that BCG efficacy depends critically on host MyD88 signalling, rather than on any single upstream pattern‑recognition receptor (8). BCG is sensed by multiple innate receptors (TLRs, IL‑1R), whose signals converge on MyD88 as a key downstream adaptor.
In MyD88‑competent hosts, BCG induces TME remodelling with iNOS⁺ inflammatory macrophages, neutrophil and CD8⁺ T‑cell expansion, and tumour regression (8). MyD88‑deficient mice mount only a blunted response with persistent tumour growth (8).
These findings identify MyD88 as a central innate signalling hub for BCG, suggesting combinations with TLR agonists and myeloid/MyD88 signatures as predictive biomarkers (8). Clinical BCG responders show similar inflamed TMEs, reinforcing MB49’s translational value (8).
While these studies provided important snapshots of the tumour microenvironment, newer MB49 derivatives have made it possible to observe immune dynamics as they unfold over time.
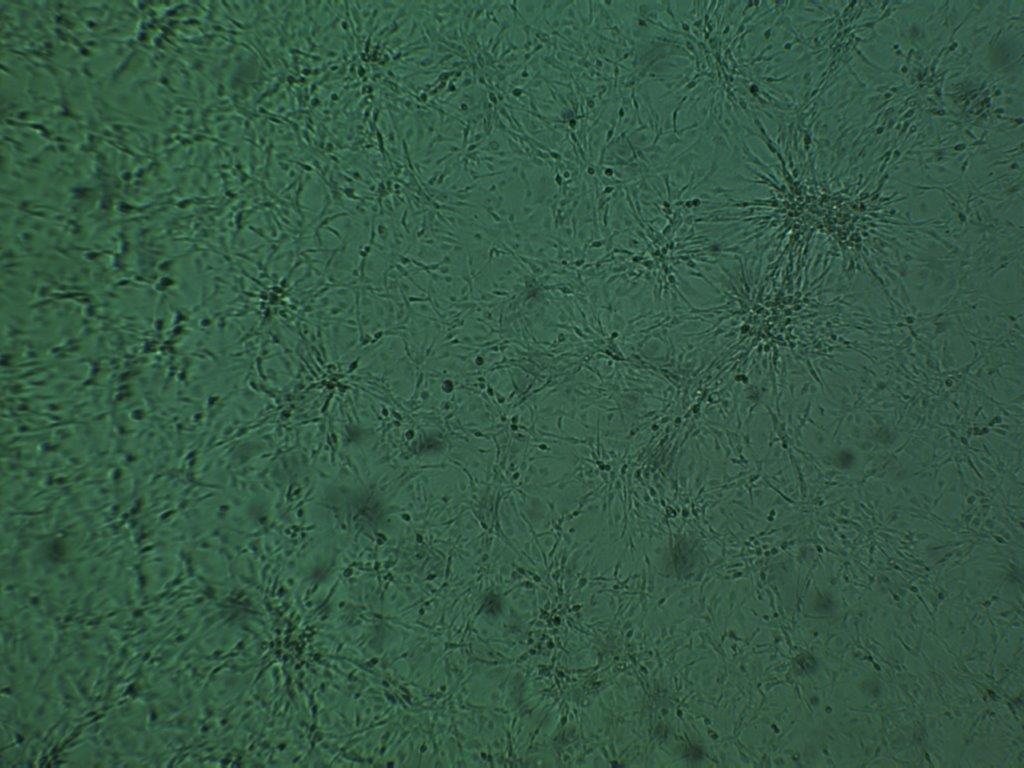
Watching the TME evolve with MB49-luc
Luciferase-expressing MB49-luc further expands MB49’s utility. It enables longitudinal, non-invasive tracking of tumour growth and immune evolution in orthotopic settings.
Early intravesical MB49-luc tumours show limited immune infiltration. Over time, bioluminescence imaging plus serial sampling reveals a sharp increase in CD45⁺ cells. These are dominated by polymorphonuclear and monocytic myeloid-derived suppressor cells (MDSCs). T-cell infiltration remains sparse, mirroring “cold” patient TMEs (4).
PD-L1 expression emerges first on myeloid cells, then tumour cells. By ~day 9, a fully established checkpoint-rich suppressive niche forms (4).
This temporal structure has direct therapeutic implications. Anti-PD-1 works well when given at peak tumour PD-L1 expression. It proves largely ineffective earlier, before checkpoint upregulation (4). Orthotopic MB49-luc therefore links TME evolution, checkpoint biology, and therapeutic timing. This is a connection few solid tumour models capture.
Why these stories matter
Together, these examples show why MB49 remains central to bladder TME research:
- Neutrophils emerge as active engineers of immune suppression
- MyD88-dependent innate sensing determines BCG success
- MB49-luc makes TME dynamics observable, not just retrospective
Few models combine this experimental flexibility with such consistent translational alignment. As new immunotherapies, combinations, and biomarkers emerge, MB49 continues delivering rigorous, interpretable insights into therapeutic mechanism.
Supporting rigorous bladder cancer research
At CancerTools, we provide original MB49 model—developed by Leonard Franks—to support reproducible, mechanism-driven research into bladder cancer immunology. Our mission is to equip academic and industry researchers with robust in vivo tools that accelerate translational insight, bridging preclinical discovery to clinical impact.
Use the MB49 and MB49-luc syngeneic models to uncover new mechanisms of immune escape and therapeutic response in bladder cancer.
References
- Summerhayes et al. 1979. J Natl Cancer Inst. 62(4):1017-1023. PMID: 107359.
- Tham et al. Clin Dev Immunol. 2011;2011:865684. Oct 13. PMID: 22013484.
- Loskog et al. 2005. Lab Anim. 39(4):384-393. PMID: 16197705.
- Domingos-Pereira S. et al. 2023 Int J Mol Sci. 23;24(1):123. PMID: 36613562.
- Bazargan et al. T Front Immunol. 2023 Oct 12;14:1275375. PMID: 37901214;
- Puttmann et al. Bladder Cancer. 2019;5(2):103-114. doi:10.3233/BLC-190219
- Jing et al. Proc Natl Acad Sci U S A. 2024 May 14;121(20):e2312855121. PMID: 38713626;
- de Queiroz N.M.G.P. et al. Sci Rep. 2021;11:15648. PMID: 34341449