The research tool: Diagnostic research tools
Professor Leigh and her team have contributed to various streams of SCC and BCC research, focusing mainly on keratinocyte biology; ranging from epithelial differentiation and the cell biology of SCC, to the molecular machinery driving non-melanoma skin cancer. Professor Leigh was a pioneer in these fields, entering research at a time when keratinocyte growth was a new technology, and was involved with producing various important antibodies and cell lines in BCC and SCC cancer identification.
We spoke with Professor Leigh and her team to delve into the importance of this stream of cancer research and what the contribution of tools can do for SCC and BCC.

The contributor
Queen Mary University of London; CRUK, London Research Institute: Lincolns Inn Fields; CRUK, London Research Institute: Clare Hall Laboratories
Non- Melanoma Skin Cancer (NMSC's) diagnostic research tools
Non-melanoma skin cancers (NMSCs or Keratinocyte cancers-KC) including basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), receive less awareness than their melanoma counterpart. This is because they are perceived as causing fewer deaths, as only SCCs metastasise. However, the incidence of NMSC is very high (18-20 times higher than that of melanoma) and there are 156,000 new non-melanoma skin cancer cases in the UK every year (2016-2018) – almost 430 every single day. Non-melanoma skin cancers commonly develop due to the skins exposure to the sun. Because these cancers are caused by excessive ultraviolet radiation, patients often end up having more than one skin cancer, resulting in multiple surgeries. Both types of carcinoma have an excellent prognosis, are slow-growing and rarely metastasise, however, in some cases they can develop into invasive skin cancers, with an aggressive nature.
It is critical to study NMSCs to produce diagnostic tests which identify high-risk tumours for metastasis and progression and generate treatments which limit carcinoma recurrence, as this is more challenging to treat.
Basal Cell Carcinoma (BCC) and Squamous cell Carcinoma (SCC)
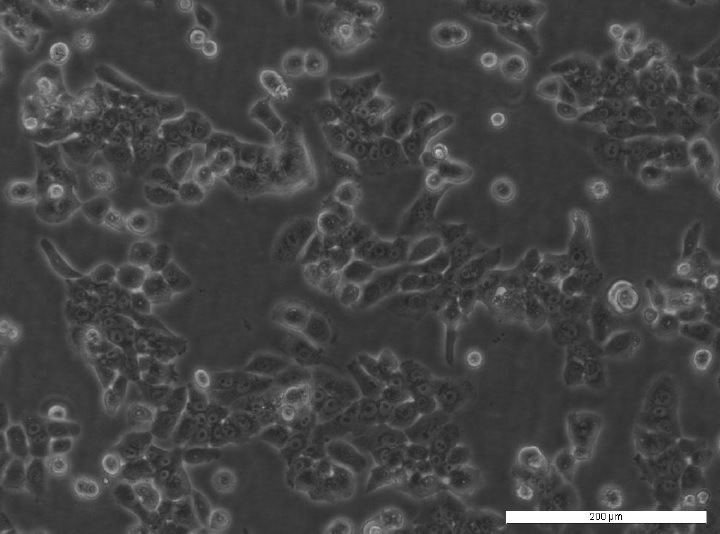
One group of patients that are significantly affected by SCC and BCC are the immunosuppressed. With over 40% of SCC mortalities occurring in organ transplant receivers, this group has an important impact on immunotherapy treatment options and survivability. In working with these patients, Professor Leigh and her team have established a unique panel of patient-derived cutaneous squamous cell carcinoma cell lines. One example from this panel is the MET1 SCC cell line.
The development of MET1 SCC cell line
This cell line was derived from a primary lesion on the hand of an immunosuppressed patient, which ultimately recurred (MET2 cell line) and metastasised (MET4SCC line), representing crucial stages in SCC transformation. Understanding the stages a squamous cell carcinoma takes in order to become increasingly invasive helps dictate preventative and therapeutic measures for this cancer. This cell line has also been used in a variety of research; from indicating HPV isn’t essential for cancerous phenotype maintenance, to furthering our understanding of epithelial-mesenchymal transition within metastasis.
Recessive Dystrophic Epidermolysis Bullosa (RBDEB)
RDEB is a debilitating condition involving a deficiency in anchoring fibrils, predominantly type VII collagen – between the epidermis basement membrane and underlying connective tissue. This leads to extremely fragile skin with severe blistering, meaning most patients develop SCC before the age of 35. Irene and her team helped to uncover the genetic basis of this condition through their research.
The development of Anti-Collagen Type VII LH7.2 antibody
Anti-Collagen Type VII LH7.2 is a monoclonal antibody which binds to an epitope of type VII collagen within the basement membrane of stratified squamous epithelia. This antibody helps diagnose RDEB as LH7.2 binding is absent or significantly reduced in RDEB patients. LH7.2 can also be used for differentiating invasive from non-invasive melanoma by assessing the integrity of epidermal basement membranes. This enables us to predict how aggressive SCC might be in RDEB patients.
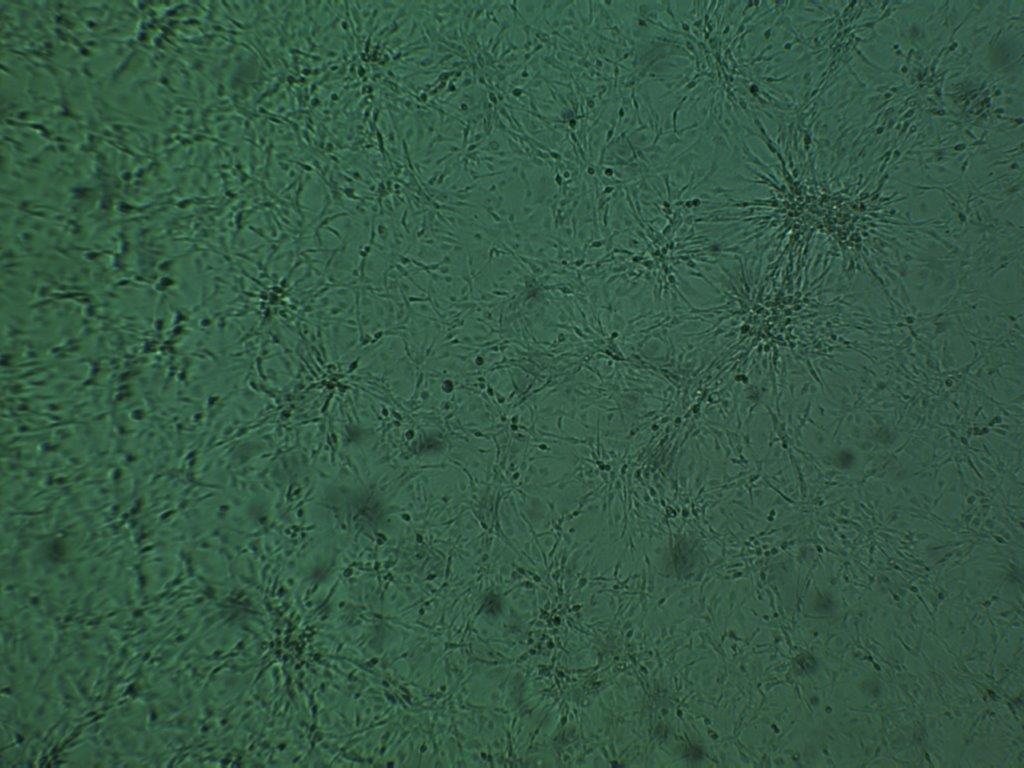
The development of Anti-Katine 5/6/18 [LP34]
Professor Leigh and her team also created a monoclonal antibody that could be used to diagnose SCC and BCC tumours. Keratins 5, 6 are members of the type II keratins family that are specifically expressed in the inner root sheath of hair follicles. Keratins demonstrate tissue and differentiation-specific expression profiles. The type II cytokeratins consist of basic or neutral proteins which are arranged in pairs of heterotypic keratin chains co-expressed during differentiation of simple and stratified epithelial tissues. Keratin 18 is a member of the type I intermediate filament chain keratin 18. Keratin 18, together with its filament partner keratin 8, are perhaps the most commonly found members of the intermediate filament gene family. These cytokeratins have been reported to be expressed in tumour cells of epithelial origin and less commonly of mesothelial origin- however, non-epithelial tumours, e.g. lymphomas, do not express these cytokeratins. Anti-Katine 5/6/18 LP34 identifies tumours with an epithelial origin and is key in pathological diagnosis and understanding metastases. As this antibody binds to keratins 5, 6 and 18, it can also be used to identify uncultured keratinocyte material. Polyspecific LP34 also has an uncommonly broad pattern of reactivity, staining all human epithelial cells – both stratified and simple epithelium.
The impact
Irene Leigh and her lab have made significant contributions to the understanding and treatment of non-melanoma skin cancers and skin diseases, generating a number of cancer research tools that can be used to diagnose these conditions. Despite the belief that these cancers are not a danger due to their high treatability and low mortality levels, investigating them can have far-reaching impacts. Understanding the common pathways between NMSCs and keratinocytes can give insight into other cancers and skin conditions. Alongside this, studying these skin cancers can lead to new novel diagnostics and therapeutics to improve cancer survival rates within at-risk populations. By contributing these research tools to the initiative, researchers globally can now utilise these tools to continue to accelerate discoveries and help grow our understanding around non-melanoma skin cancers.
”Not only do we need to be able to diagnose patients more accurately, we also need to search for clues for their treatment. This could come from a variety of sources, but you need the right reagents to do so
Professor Irene Leigh