Introduction
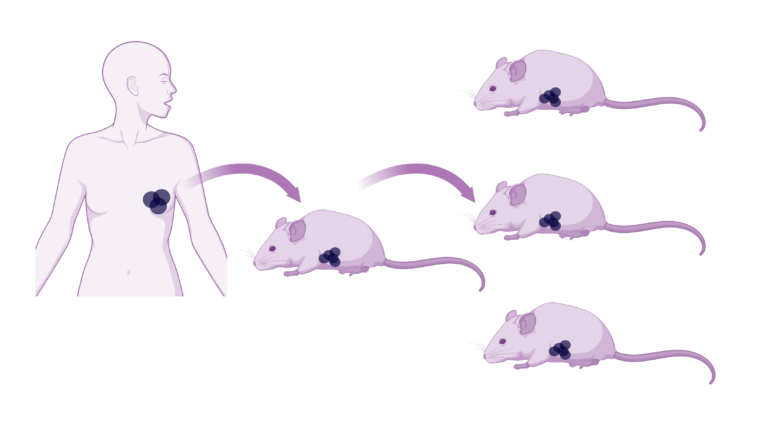
Researchers are constantly seeking novel translational tools to better model the complexity of breast cancer. Amongst these innovations, Patient-Derived Xenograft (PDX) models have emerged, as a leading breast cancer in vivo system, to study the intricacies of cancer biology. PDX models are created by transplanting human tumour tissue into immunodeficient mice, enabling breast cancer research within a more physiologically relevant environment.
At the forefront of this field, is Professor Alana Welm, based at the University of Utah’s Huntsman Cancer Institute. We met up with her to discuss her group’s groundbreaking research.

Image: Prof. Alana Welm
Journey into breast cancer research
Professor Welm’s journey into breast cancer research began after her PhD, with a desire to make an impact on human health. She explains:
“I wanted to do some research that was more directly applicable to human health. And so, for my postdoc, I joined J. Michael Bishop’s laboratory in UCSF, where I got to learn a lot about oncogenes and started working on breast cancer metastasis.”
Here, she discovered the difficulties in studying metastatic disease.
“One of the challenges I realised, was that human breast cancer cell lines are poorly metastatic. This is why I set out to make PDX models.”
Professor Welm hypothesised that growing these cancer cells in vivo, as opposed to on plastic, might enable a “metastatic memory” in the cells, or allow them to “interact with their environment in a more physiologically relevant way.”
Pioneering complex breast cancer PDX models at the Huntsman Cancer Institute
In 2007, Professor Welm established her own laboratory at the University of Utah’s Huntsman Cancer Institute and began developing novel breast cancer PDX models. These spanned different breast cancer types. Her research focuses on solving the problem of breast cancer metastasis, using in vivo PDX modelling of complex and heterogeneous breast cancers.
Professor Welm’s group have generated a large biobank of PDX models that represent breast cancer patients affected by the most advanced, and lethal forms of the disease. This includes aggressive, metastatic, and treatment resistant subtypes, providing a truer representation of the entire spectrum of disease than previously available.
Capturing the complexity of Breast Cancer
Professor Welm’s work focuses on the importance of studying metastatic disease, the killer in breast cancer. She endeavours to make sure her models are representative of metastatic disease and highlights the challenges faced and strategies used to ensure this.
“We try really hard to make sure that our models are representative of metastatic disease, but it is hard to get metastatic samples from patients… What we really try to get are the pairs, primary metastatic pairs or longitudinal samples, because then people could use them to study how the tumour evolves in the patient or how it evolves resistance to therapies.”.
These matched samples provide researchers with the tools needed to study the biology underpinning metastases.
In addition to representing metastatic disease, Professor Welm and her team have worked hard to capture the spectrum of disease experienced across breast cancer. When asked about key subsets in her collection, she notes:
“I think a really unique set are the oestrogen-receptor positive (ER+) tumours, because they are harder to grow, so there are only a few of them. We characterise all of them for their oestrogen dependence”.
She then explains that the collection also includes:
“models of ER+ breast cancer with naturally occurring mutations in the oestrogen receptor, which occurs in humans with hormone therapy”.
The biobank also contains a vast collection of triple-negative breast cancer (TNBC) models, which is essential. Professor Welm explains further:
“TNBC is a vastly heterogeneous subtype. It’s really the absence of a subtype, I guess. And we need a lot of those as well to just represent human breast cancer.”
Unlocking unexpected discoveries using these models
Professor Welm shared with us one of her most unexpected discoveries from using these PDX models:
“I think the biggest finding that we didn’t expect, was that the ability to generate a PDX model, actually predicted distant recurrence for TNBC patients. That was a complete accident. It’s like a functional test for aggressivity”.
This discovery led to further innovations, Professor Welm explains:
“It inspired our functional precision oncology trials; we knew these patients would have a bad outcome and yet we were growing their tumours. So, we thought we need to do something about this.”
This work evolved into developing matching organoids for higher throughput in vitro drug screening, enhancing the potential for personalised treatment responses.
Advancing Breast Cancer Research through collaboration
When asked about her goals for implementing PDX models in breast cancer research, Professor Welm emphasised the importance of addressing unmet clinical needs.
“Well, I think for us, the goal is to use these models to research areas of the greatest medical need in breast cancer, which are the recurrent drug-resistant metastatic tumours. There are a lot of primary tumours that we could study, we could make models of, but those might not represent the disease where we need to make new therapies.”
We are very grateful to Professor Welm for sitting down with us to discuss her work and PDX models in more detail. Professor Welm has deposited 53 of these PDX models with the CancerTools.org biorepository. This partnership aims to further accelerate breast cancer research, drug discovery, and precision oncology, by making these cancer research tools more accessible to the global research community.
These models offer researchers unprecedented opportunities to study breast cancer metastasis, drug resistance, and tumour evolution in a physiologically relevant context, paving the way for more effective treatments and better outcomes.